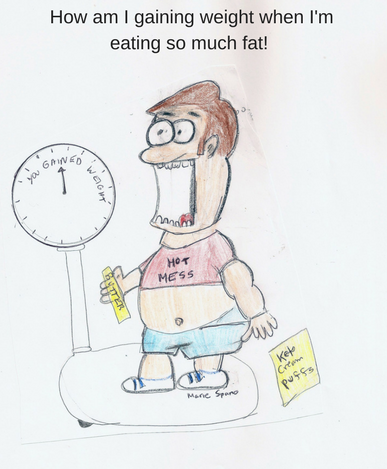
Ketogenic Diets: Eating Fat Won’t Make You Thin
Following a ketogenic diet will not guarantee weight loss. Producing a lot of ketones does not mean you are shredding body fat. Gulping down shots of olive oil or putting butter in your coffee won’t make you thin. You must consume fewer calories than you need, over time, to lose body fat. This blog post will cover: What is Ketosis? Eating fat Makes You Burn More Fat for Energy but… Who is this Diet Good For? Who Should Avoid the …